As winter settles in, there is an accompanying rise in the prevalence of Seasonal Affective Disorder (SAD), a form of depression that occurs typically during the late fall and winter months. When daylight hours shorten in the winter, disruptions to our internal clocks occur, impacting the production of mood-regulating neurotransmitters like serotonin. Substantial research and clinical experience point to bright light therapy as an effective non-invasive treatment for seasonal depression. Light therapy, also known as phototherapy, involves exposure to a bright light that mimics natural sunlight. The science behind this therapy is rooted in its ability to regulate circadian rhythms and influence neurotransmitter levels. Research has shown that just 20 to 30 minutes of daily exposure to bright light (10,000 lux) can lead to notable improvements in mood, energy levels, and sleep patterns. This makes light therapy a valuable option for those seeking relief from the winter blues. A large number of light boxes are available on the market, but it can be difficult to know which of those meet the specifications researched for effective treatment of seasonal depression. Light boxes aren't regulated by the Food and Drug Administration (FDA) for SAD treatment, so it's important to understand your options. The Yale School of Medicine provides helpful information and links to specific light boxes that have been demonstrated to be effective. Consistency is essential for maximizing the benefits of light therapy. Whether using it while enjoying a morning coffee, catching up on emails, or reading, integrating light therapy into these activities can make it a seamless part of your daily life.
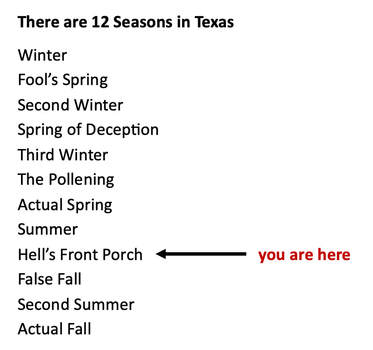
Consult with a healthcare professional to determine if you are a good candidate for light therapy, obtain any individualized recommendations, and discuss any pre-existing eye conditions or medications that may be affected by light exposure. Note that light therapy is not recommended for patients with retinal diseases including macular degeneration, or diseases such as diabetes which may be associated with retinal disease. Light treatment must be monitored with particular caution in individuals with bipolar disorders. It is recommended that light therapy be done under the supervision of a clinician qualified to treat mood disorders. Additional research and information on light therapy can be found by following the links below: Mayo Clinic Harvard School of Public Health National Institutes of Health Yale School of Medicine Dallas is currently in the midst of another triple digit heatwave that, despite the no-doubt immanent arrival of pumpkin-spice season, shows no signs of letting up soon. While there are regular reminders in the news to guard against heat stroke and the physical effects of heat, it is also important to know that extreme heat can negatively impact our mental health as well. A recent meta-analysis published in The Lancet found positive associations between temperature and suicide rates, hospital admissions for mental illness, and community mental health outcomes. Aggression, domestic violence, and substance use can also increase during periods of extreme heat. Certain groups are more vulnerable to the mental health impacts of extreme heat. People with pre-existing mental health conditions, dementia, or those taking certain medications (more on that below) might be at higher risk. Socioeconomic factors, such as poverty and substance use disorders, also substantially contribute to vulnerability. Certain classes of medication used to manage physical health conditions can make it harder for your body to handle extreme heat. These include medications to treat heart conditions, blood pressure, diuretics, anticholinergics (such as those prescribed for Parkinson’s and overactive bladder), antihistamines, and decongestants.
Similarly, some medications used to manage mental health conditions can impact the body's ability to stay hydrated, regulate temperature, and respond to heat. These include central nervous system stimulants prescribed for ADD/ADHD, medications to treat depression and anxiety (SSRIs, SNRIs, and tricyclic antidepressants), as well as some medications prescribed for schizophrenia and bipolar disorders. These medications can be life-saving and have profound benefits for quality of life, so it is important for healthcare providers and patients to work together to manage medications effectively, especially during heatwaves or other extreme weather events. As we collectively navigate the extreme heat of the next several weeks, you can prioritize your physical and mental health by staying well-hydrated, taking precautions against becoming overheated, and checking on vulnerable family members, friends, and neighbors. If you'd like to learn more about the Lancet study, Dr. Robert Bright, a psychiatrist with the Mayo Clinic, talks more about that research and the effects of heat on mental health here. This video, developed by the Trauma Foundation, gives a helpful overview of how trauma and chronic stress affects our nervous system and how those effects impact our health and well-being. The content is largely based on Dr. Stephen Porges research on Polyvagal Theory. You can learn more about Polyvagal theory here. Research has shown physical movement to be a powerful tool in alleviating symptoms of depression and anxiety, as well as enhancing our overall sense of well-being. As we enter the sunshine and blue skies of Hot Texan Summer (TM), it is helpful to remember the beneficial effects of movement on our mental health and the importance of incorporating physical activity into our daily lives.
Over the years, a growing body of research has shed light on the positive impact of physical activity on individuals experiencing depression and anxiety. These studies highlight several key findings: Release of Mood-Boosting Chemicals. Engaging in regular physical activity triggers the release of endorphins, neurotransmitters that act as natural painkillers and mood elevators. Endorphins induce feelings of happiness and well-being, counteracting negative emotions. This chemical boost can significantly improve mood and reduce symptoms of anxiety. Neurogenesis and Neuroplasticity. Movement has been shown to promote neurogenesis (the formation of new neurons) and enhance neuroplasticity (the brain's ability to reorganize and adapt). These processes play a vital role in improving cognitive function, memory, and learning abilities. By stimulating the growth and connectivity of brain cells, physical activity helps create a healthier neural network that supports mental well-being. Studies indicate that regular exercise may even significantly reduce the risk of developing dementia. Stress Reduction and Anxiety Management. Movement acts as a natural stress reliever by reducing the levels of stress hormones such as cortisol and promoting relaxation. Regular activity can also help manage anxiety symptoms, which often coexist with depression. Engaging in activities like walking, jogging, yoga, or swimming can provide a much-needed respite from daily stressors, promote a sense of calm and mental clarity, and improve sleep. Social Interaction and Support. Participating in group activities or team sports provides an opportunity for social interaction and support. Engaging in activity with others can foster a sense of belonging and community, creating a supportive environment that combats loneliness and enhances our sense of well-being. Physical activity can be a powerful a complementary tool alongside professional treatment for depression and anxiety. A recent meta-analysis published in JAMA Psychiatry, found that relatively small doses of even moderate physical activity (2 hours per week) were associated with substantially lower risks of depression. (Dr. Roger Seheult examines this and another recent study exploring depressive symptoms and sedentary behavior in adolescence in the video linked below.)  Photo by Christian Bowen on Unsplash Physical activity can be a powerful a complementary tool alongside professional treatment for depression and anxiety. A recent meta-analysis published in JAMA Psychiatry, found that relatively small doses of even moderate physical activity (just 2 total hours per week) were associated with substantially lower risks of depression. (Dr. Roger Seheult examines this and another recent study exploring depressive symptoms and sedentary behavior in adolescence in the video linked below.) If you are looking to enjoy these benefits by adding more movement into your life, here are some helpful tips: Find or Rediscover the Joy of Movement. Experiment with different forms of movement until you find activities that you enjoy. Whether it's walking through the neighborhood, learning a TikTok dance, hiking with friends, hula-hooping, kayaking, or playing pickleball, choosing activities you genuinely enjoy will increase the likelihood of incorporating them into your regular routine. Seek Support and Connection. Consider involving a friend or family member, or joining a club, exercise group or class to provide support and accountability. Sharing activity with others can make it more enjoyable, which will help you want to return to it regularly. Movement can be a powerful ally in supporting our mental health and overall well-being. By engaging in physical activity, we tap into natural mood-boosting chemicals, promote brain health, and cultivate social connections. Embracing joyful movement as part of our daily life empowers us to take an active role in our mental health, helping us on the path towards a healthier, happier life. Now, please excuse me as I take my not-so-stupid walk. (I hope to see you out there.) This article by Scott Berinato of the HBR explores the different types of grief we are collectively experiencing in the face of this pandemic. There is a storm coming. There’s something bad out there. With a virus, this kind of grief is so confusing for people. Our primitive mind knows something bad is happening, but you can’t see it. This breaks our sense of safety. We feel the world has changed, and it has. We know this is temporary, but it doesn’t feel that way, and we realize things will be different. Just as going to the airport is forever different from how it was before 9/11, things will change and this is the point at which they changed. The loss of normalcy; the fear of economic toll; the loss of connection. This is hitting us and we’re grieving. Collectively. Finding ways to name what we are feeling, to speak it and ask for help, empowers us to experience and then move through the emotion. As the David Kessler states in the interview, “Emotion needs motion.” Kessler suggests grounding and mindfulness techniques to help calm overwhelming anxiety and re-center ourselves in the present and on the aspects of this situation which we can control.
As the number of cases of COVID-19 increase, so does our collective anxiety. It can be difficult to know what tomorrow, next week, or next month will bring. This lack of expectations and being unable to plan can heighten anxiety. Routines we may have worked hard to build and which support our work-life balance and mental health are thrown off. And many of us find ourselves isolated from our usual social supports. In the video below, clinical psychologist Dr. Alli Mattu addresses important coping skills for working from home, social distancing without feeling isolated, and managing information related to the COVID-19 public health crisis without feeling overwhelmed. The following additional resources can help individuals and communities navigate this stressful time. Remember, we're all in this together. CDC: COVID-19 Resources Latest updates, tips and resources by the US Centers for Disease Control. Living With Mental Illness During COVID-19 Outbreak– Preparing For Your Wellness This webpage provides information and wellness tips for individuals living with mental health conditions during the COVID-19 outbreak. Mental health and wellness during a public health crisis Dr. LaGenia Bailey, a former DBSA board member, discusses tips on how to stay well during this public health crisis. In this podcast, she addresses the benefits of mindfulness practice, lifestyle habits, and ways to stay connected with others to avoid isolation. COVID-19 Mental Health Support Line: 833-986-1919 Texas Health and Human Services has launched a 24/7 statewide mental health support line to help Texans experiencing anxiety, stress or emotional challenges due to the COVID-19 pandemic. People can call the Statewide COVID-19 Mental Health Support Line 24 hours a day, 7 days a week toll-free at 833-986-1919. Operated by the Harris Center for Mental Health and IDD, the support line offers trauma-informed support and psychological first aid to those experiencing stress and anxiety related to COVID-19. Seven Crucial Research Findings that can Help People Deal with COVID-19 Psychological research on past crises can help people cope with the daily — sometimes hourly — news flashes about the coronavirus. How to Transition to Seeing Your Therapist Online Continue the work of therapy even from a distance. (And yes, Dr. Novinski offers sessions via Telehealth.) Psychologists’ Advice for Newly Remote Workers As employers close offices to slow the spread of COVID-19, here’s advice from I/O psychologists on how both managers and employees can work more effectively during this time. Dial 2-1-1 If you need assistance finding food, paying for housing bills, accessing free childcare, or other essential services, visit 211.org or dial 211 to speak to someone who can help. Run by the United Way. COVID-19 Ancillary Costs The HealthWell Foundation announced a COVID-19 Fund that provides up to $250 in assistance with ancillary costs associated with COVID-19. Grants awarded through the fund will provide reimbursement assistance to at risk or quarantined individuals for delivered food, medication, telehealth copays and transportation costs associated with COVID-19. Care for your Coronavirus Anxiety Staying Grounded Meditations and Calming Exercises National Domestic Violence Hotline For any victims and survivors who need support, call 1-800-799-7233 or 1-800-799-7233 for TTY, or if you’re unable to speak safely, you can log onto thehotline.org or text LOVEIS to 22522. Talking to Kids about the Coronavirus The Parent Guide to Resilience Yale University's The Science of Well-Being Yale's most popular class is now free online via Coursera. The course focuses on how to increase happiness and productivity in your everyday life. University of Pennsylvania: Positive Psychology Resilience Skills I often say that the importance of sleep should be covered in Volume 1 of So You've Decided to go to Therapy. The link between sleep and mood has been seen over and over in research. People with insomnia are 10 times as likely to have clinical depression and 17 times as likely to have clinical anxiety as those who sleep normally. We have long known that sleep difficulties are symptomatic of depression, anxiety, and other mental health conditions. New research is revealing that the relationship between sleep and our physical and mental health is much more complex -- and malleable. For example, the more a person experiences difficulty sleeping and the more frequently they wake at night as a result, the higher the chances of developing depression even if they did not struggle with depression before. More research is being conducted on factors that contribute to difficulty falling and staying asleep, or to shifting nighttime routines. Many studies have explored the connection between screen time (i.e., blue light exposure) and sleep difficulties. The readily available connection to work, social connections, entertainment, and distraction that come from our computers and phones carries with it implications for our sleep and thereby our physical and mental health. Some clever IT professionals and start-ups have found a way to turn technology in our favor when it comes to sleep. Apps like Headspace and Calm have skyrocketed to the top of the Apple App and Google Play stores, due in no small part to their audio features that aid users in falling and staying asleep. If you find that you struggle with getting good quality sleep, consider these sleep hygiene recommendations from the National Sleep Foundation:
Think about (or discuss in therapy!) ways in which you can actively work to prioritize your sleep to help improve your physical and mental health.
As psychologist Guy Winch explains, "Much as accountants' busiest time of year is tax season in April, we therapists see our practices overflow in November and December. Why? ‘Tis the season of family gatherings."
Family gatherings have the potential to help us feel connected and loved, but even within the best of family dynamics, cooking, cleaning, and coordinating schedules can be stressful. And the fact of the matter is that not every family shares the best dynamics on display in Hallmark Holiday Specials. Family gatherings can bring old wounds to the surface, and leave many feeling less connected, less understood, and alone despite the holiday crowds. For those who live far from family and friends, singles, and those who are newly separated, divorced or grieving, the family-focused holidays can be a painful and lonely time. Add these factors to the days getting shorter, the weather colder, spending less time outdoors in the sun, and it is easy to understand how the holidays can leave us feeling stressed out and blue. The following resources can help you survive and thrive through this holiday season:
If you find yourself feeling overwhelmed with stress or sadness, know that you are not alone. Talking with a therapist about coping with the holidays specifically, or untangling long-standing relationship patterns, can be useful and help you move through the holidays and into the new year with less stress, more understanding of yourself and others, and more skills to navigate this time of year with more grace and less stress in the future. Heads Together is a UK campaign, spearheaded by the Duke and Duchess of Cambridge and Prince Harry to end stigma around mental health. This week the campaign released a video of the Duke, Duchess and Prince discussing their support of the mental health initiative. The Heads Together campaign has partnered with this weekend's London Marathon to help raise awareness and encourage people to speak up about and prioritize their mental health (all the runners will be given Heads Together headbands, modeled by the Royal Family above). “Since we launched Heads Together last May, we have seen time and time again that shattering stigma on mental health starts with simple conversations. When you realise that mental health problems affect your friends, neighbours, children and spouses, the walls of judgement and prejudice around these issues begin to fall. And we all know that you cannot resolve a mental health issue by staying silent." Here in the US, the OK to Say campaign has been working to encourage people to talk openly about mental health. So often people do not ask for or seek out the help that they need because of stigma. Sharing our stories and working as a community to encourage one another and share resources can improve and save lives.
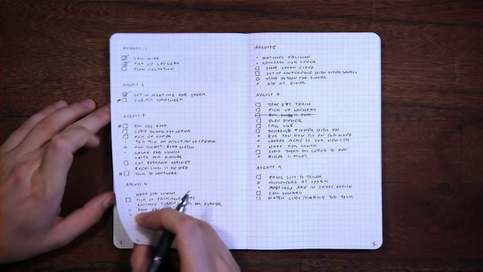
If you are interested in continuing this conversation and showing your support, consider joining the National Alliance on Mental Illness (NAMI) annual Dallas NAMI Walks 5k coming up in on May 13. Journaling can be an invaluable resource for therapy. When someone describes an unusually good (or bad) day in session, I often ask them to reflect on what was different. Answers of "I don't know." or "Nothing, I think." are supremely frustrating in that they leave a person feeling helpless, as though a good or bad day comes out of the blue or passes them by completely outside of their control. More often than not, there are concrete things someone did, thought, or felt that either contributed to a better day or perhaps kept a bad day or experience from "taking over" or becoming unmanageable. Take for example the few pounds we all may or may not have added over the holidays. We can be perplexed when we look at the scale now and wonder, "How did that happen?" But we also know that people who log everything that they eat or drink 1) tend to eat and drink more mindfully and healthily, and 2) can readily identify that pumpkin cheesecake or second helping that likely added to the scale come January. Journaling can provide that level of insight for your mental health. Identifying patterns can be empowering and can provide you with your own individual data on what works, and what doesn't, what contributes to a great week, and what behaviors, skills, and experiences help you nip anxiety or depression in the bud. This process can help you clarify thoughts and feelings and solve problems more effectively. Journaling can improve your body as well as your mind. University of Texas social psychologist and researcher, James Pennebaker has found that regular journaling strengthens immune cells (lymphocytes). A study published in Advances in Psychiatric Treatment noted improvements in both physical and psychological health in clinical and non-clinical groups after just 3-5 15-20 minute journaling sessions. Other research suggests that journaling offers not just emotional, but physical benefits to individuals battling terminal or life-threatening illnesses. Perhaps we see these benefits because, as Pennebaker suggests, writing about stressful events helps you come to terms with them and reduces the impact of these stressors on your physical health. Remind you of therapy? Journaling and therapy can beautifully complement one another. The work that you do journaling over the week can build on the momentum, insights, and positive changes you are developing in therapy. How to begin? When many people hear "journal," the embarrassing teenage diary tucked away in a sock drawer comes to mind. But a journal can be much more than a diary (or much less, if you like), and there as many ways to keep a journal as there are journal-ers. For those who don't fancy themselves writers, or who feel overwhelmed at where to begin, the Bullet Journal developed by Ryder Carroll offers a streamlined way of tracking daily activities, including mental health. What to journal? In addition to logging events and experiences, a journal can be used to track moods, how you feel physically (e.g., energy level, headaches), behaviors that can affect your mental and physical health (e.g., sleep, exercise, taking vitamins and medications), and self-care (e.g., socializing, meditation). Tracking can provide valuable data and trends to discuss in therapy. You may also find it useful to include post-therapy session notes (e.g., insights, reminders, topics to discuss or come back to next session). Adding space for a gratitude journal can provide time and space to reflect on positive thoughts, feelings, and experiences in a way that can actually help re-train your brain to more readily identify (rather than discount) positive experiences. Including self-care ideas for when you notice triggers or early signs of depression or anxiety can help you easily identify tried and true methods to change course or help manage those negative feelings before they become overwhelming. Here are some additional tips to get you started:
Make it yours. Your journal can be as minimalistic and straightforward or artistic and detailed as you want. Are you the type of person (this month) who delights in a To Do list? Or does a listing these tasks and obligations bring you additional stress? If so, you may find you are better served by a "Done" list. Find your own style and what works best for you. The beauty of making a journal your own is that it can change with you from week to week, and month to month. Build on what works for you, and leave what does not behind without guilt (recognizing each of these is progress in and of itself!). Finally, I'm personally a proponent of putting pen to paper. One of the benefits of a journal that you physically create yourself is that you have complete control in customizing it to fit your needs as opposed to having pre-printed pages that you don't love or use in a day planner or maintaining multiple tracking apps. That said, if a physical journal just feels too analog for your life, there are a number of apps out there that track habits, moods, and provide space for journaling. Just be aware of protecting your privacy and online presence if you choose a digital route. Happy journaling! Additional Journaling Resources: BulletJournal.com offers a videos, tips, and tutorials on how to start a bullet journal. Rachel Wilkerson Miller and Anna Borges at Buzzfeed offer a lighthearted and insightful collection of ways to use journaling to track and improve your mental health. Steven Stosney at Psychology Today, describes the research on the results of journaling and gives tips for reaping the benefits of journaling while avoiding the pitfalls. |
About the AuthorClinical psychologist Dr. Kristy Novinski contributes insights, book and film reviews, discussions of pop culture, and exploration of news and research in the field of psychology. What I'm Reading
Categories
All
|
Las Colinas Psychological Services, PLLC |
© 2023 Las Colinas Psychological Services, PLLC. All rights reserved.
|









 RSS Feed
RSS Feed