As winter settles in, there is an accompanying rise in the prevalence of Seasonal Affective Disorder (SAD), a form of depression that occurs typically during the late fall and winter months. When daylight hours shorten in the winter, disruptions to our internal clocks occur, impacting the production of mood-regulating neurotransmitters like serotonin. Substantial research and clinical experience point to bright light therapy as an effective non-invasive treatment for seasonal depression. Light therapy, also known as phototherapy, involves exposure to a bright light that mimics natural sunlight. The science behind this therapy is rooted in its ability to regulate circadian rhythms and influence neurotransmitter levels. Research has shown that just 20 to 30 minutes of daily exposure to bright light (10,000 lux) can lead to notable improvements in mood, energy levels, and sleep patterns. This makes light therapy a valuable option for those seeking relief from the winter blues. A large number of light boxes are available on the market, but it can be difficult to know which of those meet the specifications researched for effective treatment of seasonal depression. Light boxes aren't regulated by the Food and Drug Administration (FDA) for SAD treatment, so it's important to understand your options. The Yale School of Medicine provides helpful information and links to specific light boxes that have been demonstrated to be effective. Consistency is essential for maximizing the benefits of light therapy. Whether using it while enjoying a morning coffee, catching up on emails, or reading, integrating light therapy into these activities can make it a seamless part of your daily life.
Consult with a healthcare professional to determine if you are a good candidate for light therapy, obtain any individualized recommendations, and discuss any pre-existing eye conditions or medications that may be affected by light exposure. Note that light therapy is not recommended for patients with retinal diseases including macular degeneration, or diseases such as diabetes which may be associated with retinal disease. Light treatment must be monitored with particular caution in individuals with bipolar disorders. It is recommended that light therapy be done under the supervision of a clinician qualified to treat mood disorders. Additional research and information on light therapy can be found by following the links below: Mayo Clinic Harvard School of Public Health National Institutes of Health Yale School of Medicine Dallas is currently in the midst of another triple digit heatwave that, despite the no-doubt immanent arrival of pumpkin-spice season, shows no signs of letting up soon. While there are regular reminders in the news to guard against heat stroke and the physical effects of heat, it is also important to know that extreme heat can negatively impact our mental health as well. A recent meta-analysis published in The Lancet found positive associations between temperature and suicide rates, hospital admissions for mental illness, and community mental health outcomes. Aggression, domestic violence, and substance use can also increase during periods of extreme heat. Certain groups are more vulnerable to the mental health impacts of extreme heat. People with pre-existing mental health conditions, dementia, or those taking certain medications (more on that below) might be at higher risk. Socioeconomic factors, such as poverty and substance use disorders, also substantially contribute to vulnerability. Certain classes of medication used to manage physical health conditions can make it harder for your body to handle extreme heat. These include medications to treat heart conditions, blood pressure, diuretics, anticholinergics (such as those prescribed for Parkinson’s and overactive bladder), antihistamines, and decongestants.
Similarly, some medications used to manage mental health conditions can impact the body's ability to stay hydrated, regulate temperature, and respond to heat. These include central nervous system stimulants prescribed for ADD/ADHD, medications to treat depression and anxiety (SSRIs, SNRIs, and tricyclic antidepressants), as well as some medications prescribed for schizophrenia and bipolar disorders. These medications can be life-saving and have profound benefits for quality of life, so it is important for healthcare providers and patients to work together to manage medications effectively, especially during heatwaves or other extreme weather events. As we collectively navigate the extreme heat of the next several weeks, you can prioritize your physical and mental health by staying well-hydrated, taking precautions against becoming overheated, and checking on vulnerable family members, friends, and neighbors. If you'd like to learn more about the Lancet study, Dr. Robert Bright, a psychiatrist with the Mayo Clinic, talks more about that research and the effects of heat on mental health here. A recent study conducted in Switzerland involving over 2,300 adults has found that leading a purposeful life can help combat loneliness. The study revealed that individuals who reported having a sense of purpose experienced less loneliness, regardless of their age.
One of the study's co-authors, While activities involving social interactions were found to provide a sense of purpose, the study emphasizes that combating loneliness goes beyond mere companionship. It was discovered that finding meaning in life becomes particularly important for older adults, especially those in their 70s and beyond, as this is a stage often associated with increased loneliness. Loneliness is known to have detrimental effects on health, cognitive decline, and even mortality. The study emphasizes that a sense of purpose, whether it involves a grand mission or a personal hobby, can offer significant protection against loneliness. It is important to note that a sense of purpose can be derived from relationships, experiences, and feeling connected to something greater than yourself. While interactions with others can contribute to a purpose-filled life, the study suggests that having a sense of purpose is effective in fighting loneliness, regardless of the number of people involved. Ultimately, finding meaning, even in seemingly ordinary experiences, can significantly contribute to a person's well-being and combat loneliness. You can read more about this study here. This video, developed by the Trauma Foundation, gives a helpful overview of how trauma and chronic stress affects our nervous system and how those effects impact our health and well-being. The content is largely based on Dr. Stephen Porges research on Polyvagal Theory. You can learn more about Polyvagal theory here. Research has shown physical movement to be a powerful tool in alleviating symptoms of depression and anxiety, as well as enhancing our overall sense of well-being. As we enter the sunshine and blue skies of Hot Texan Summer (TM), it is helpful to remember the beneficial effects of movement on our mental health and the importance of incorporating physical activity into our daily lives.
Over the years, a growing body of research has shed light on the positive impact of physical activity on individuals experiencing depression and anxiety. These studies highlight several key findings: Release of Mood-Boosting Chemicals. Engaging in regular physical activity triggers the release of endorphins, neurotransmitters that act as natural painkillers and mood elevators. Endorphins induce feelings of happiness and well-being, counteracting negative emotions. This chemical boost can significantly improve mood and reduce symptoms of anxiety. Neurogenesis and Neuroplasticity. Movement has been shown to promote neurogenesis (the formation of new neurons) and enhance neuroplasticity (the brain's ability to reorganize and adapt). These processes play a vital role in improving cognitive function, memory, and learning abilities. By stimulating the growth and connectivity of brain cells, physical activity helps create a healthier neural network that supports mental well-being. Studies indicate that regular exercise may even significantly reduce the risk of developing dementia. Stress Reduction and Anxiety Management. Movement acts as a natural stress reliever by reducing the levels of stress hormones such as cortisol and promoting relaxation. Regular activity can also help manage anxiety symptoms, which often coexist with depression. Engaging in activities like walking, jogging, yoga, or swimming can provide a much-needed respite from daily stressors, promote a sense of calm and mental clarity, and improve sleep. Social Interaction and Support. Participating in group activities or team sports provides an opportunity for social interaction and support. Engaging in activity with others can foster a sense of belonging and community, creating a supportive environment that combats loneliness and enhances our sense of well-being. Physical activity can be a powerful a complementary tool alongside professional treatment for depression and anxiety. A recent meta-analysis published in JAMA Psychiatry, found that relatively small doses of even moderate physical activity (2 hours per week) were associated with substantially lower risks of depression. (Dr. Roger Seheult examines this and another recent study exploring depressive symptoms and sedentary behavior in adolescence in the video linked below.)  Photo by Christian Bowen on Unsplash Physical activity can be a powerful a complementary tool alongside professional treatment for depression and anxiety. A recent meta-analysis published in JAMA Psychiatry, found that relatively small doses of even moderate physical activity (just 2 total hours per week) were associated with substantially lower risks of depression. (Dr. Roger Seheult examines this and another recent study exploring depressive symptoms and sedentary behavior in adolescence in the video linked below.) If you are looking to enjoy these benefits by adding more movement into your life, here are some helpful tips: Find or Rediscover the Joy of Movement. Experiment with different forms of movement until you find activities that you enjoy. Whether it's walking through the neighborhood, learning a TikTok dance, hiking with friends, hula-hooping, kayaking, or playing pickleball, choosing activities you genuinely enjoy will increase the likelihood of incorporating them into your regular routine. Seek Support and Connection. Consider involving a friend or family member, or joining a club, exercise group or class to provide support and accountability. Sharing activity with others can make it more enjoyable, which will help you want to return to it regularly. Movement can be a powerful ally in supporting our mental health and overall well-being. By engaging in physical activity, we tap into natural mood-boosting chemicals, promote brain health, and cultivate social connections. Embracing joyful movement as part of our daily life empowers us to take an active role in our mental health, helping us on the path towards a healthier, happier life. Now, please excuse me as I take my not-so-stupid walk. (I hope to see you out there.) Social Media Health RecommendationsThis spring a presidential panel of the American Psychological Association (APA) has produced recommendations for the use of social media by adolescents. The advisory panel was formed to provide recommendations grounded in research to ensure that adolescents develop healthy social media practices. The result is the American Psychological Association Health Advisory on Social Media Use in Adolescence. The report notes that while these platforms can promote healthy socialization, their use should be preceded by training in social media literacy to ensure that children and teens have skills that will maximize the chances for balanced, safe and meaningful experiences. This report notes that social media use is not inherently beneficial or harmful to young people. The effects of social media depend on adolescents' personal and psychological characteristics, social circumstances, and the specific content, features, or functions they encounter on social media platforms. The report emphasizes that not all findings apply equally to all children and teens. Scientific findings should be used in conjunction with knowledge of specific kids’ strengths, weaknesses, developmental maturity, and contexts to make decisions tailored to each individual.  Photo by Laura Chouette on Unsplash In addition to the new report, the APA's chief science officer, Dr. Mitch Prinstein, provides Q&A and recommendations for parents on how to help teens develop social media literacy skills. Dr. Prinstein specifically advises parents to:
You can read the APA's recommendations in full here, and Dr. Prinstein's Q&A here. Dr. Dara Greenwood, social psychologist and associate professor of Psychology at Vassar College, provides a thoughtful and engaging article interweaving psychological research with powerful messages from Disney's Encanto that are resonating with children and adults. Greenwood's key take-aways:
Check out the full article here.
Are you looking for some good distractions to help manage your 2020/COVID/quarantine/election/end-of-daylight-savings/holiday stress? These are a few of the things that have helped to keep my mind occupied and my heart hopeful. BooksDaniel J. Levitin's Successful Aging: A Neuroscientist Explores the Power and Potential of Our Lives. “Growing old may be the only event in life that is both desired and feared. Daniel Levitin alleviates the fear with sound advice that can tilt the balance so that we have more healthy years and fewer sick ones. The brilliance of this book is that Levitin not only tells us what to do and what not to do—he gracefully and eloquently shares the science behind how we can change our minds and brains, and how even small changes can reap large benefits. Share this book—especially with anyone you hope to grow old with.” -Diane Halpern, past-president of the American Psychological Association Lori Gottlieb's Maybe You Should Talk to Someone: A Therapist, Her Therapist, and Our Lives Revealed. "[In the end, Gottlieb and her patients] are more aware—of themselves as people, of the choices they’ve made, and of the choices they could go on to make . . . It’s exploration—genuinely wanting to learn answers to the question Why am I like this?, so that maybe, through better understanding of what you’re doing, you figure out how to be who you want to become." -Slate Mark O'Connell's Notes from the Apocolypse: A Personal Journey to the End of the World and Back. "A fitting travelogue for our stationary moment...O’Connell’s 'future-dread' haltingly yields to faith in humanity’s resilience, resourcefulness, and capacity for cooperation." - New Yorker Allie Brosch's Solutions and Other Problems. “Gut-busting . . . . Like a millennial James Thurber, Brosh has a knack for seeding a small, choice detail that snowballs into existential chaos . . . [Her] spidery and demented digital portraits, a visual expression of fun-house mirror anxiety, fits her material perfectly. . . This achingly accurate and consistently hilarious comic memoir finds Brosh moving forward and becoming a stronger, braver storyteller page by page.” - Publishers Weekly, Starred Review Dan Rather's What Unites Us: Reflections on Patriotism. “…a deeply felt reminder of what is the best of America. What Unites Us is at times almost unbearably poignant. Yet Rather’s words provide a sort of salve—and clear thinking about how to recover from these ugly times. What Unites Us is a passionate treatise on preserving the best of America and letting go of that which makes us weaker.” - BookPage Gail Honeyman's Eleanor Oliphant is Completely Fine. “Eleanor Oliphant is endearing, [a] whip-smart read. . . a fascinating story about loneliness, hope, tragedy and humanity. Honeyman’s delivery is wickedly good, and Eleanor won’t leave you anytime soon." - Associated Press MoviesRotten Tomatoes guide to 150 Great Feel-Good Movies You can Stream Right Now. (Note that the better reviewed films come latest in the list.) Empire's list of 30 Feel Good Movies to Distract You from the Horror of 2020. Some never-fail feel-good films include: Singin' in the Rain Spider-Man: Into the Spider-Verse The Greatest Showman Paddington (1 and 2, actually) and The Princess Bride. SeriesThe Great British Baking Show (Netflix) may help restore your faith in humanity. With its British charm and contestants who root for one another and take both their wins and losses on the chin, the annual baking competition is feel-good TV at its best. The Mandalorian (Disney+). Jon Favreau's Disney Original series is an exquisitely shot gun-slinger Western set in the cinematic universe of Star Wars. Also, Baby Yoda. Need I say more? Ted Lasso (Apple TV+). Ted Lasso (played by Jason Sudeikis) is an American football coach hired as the unlikely coach for an English premier league football (soccer) club, is definitely less family-friendly, but 100% wholesome with some of the best quote-able quotes to come out of 2020. A World of Calm (HBO Max). This series of 30-minute documentaries comes from the creators of one of the most popular mediation apps, Calm. One person described an episode to me as "a nature documentary about a sea turtle - except that unlike a nature documentary, the sea turtle in A World of Calm is never in peril!" This page contains links to websites not administered by Las Colinas Psychological Services (LCPS). LCPS is not responsible or liable for the accuracy or the content of linked pages. LCPS does not benefit from the sale or promotion of the organizations, books, or websites listed above.
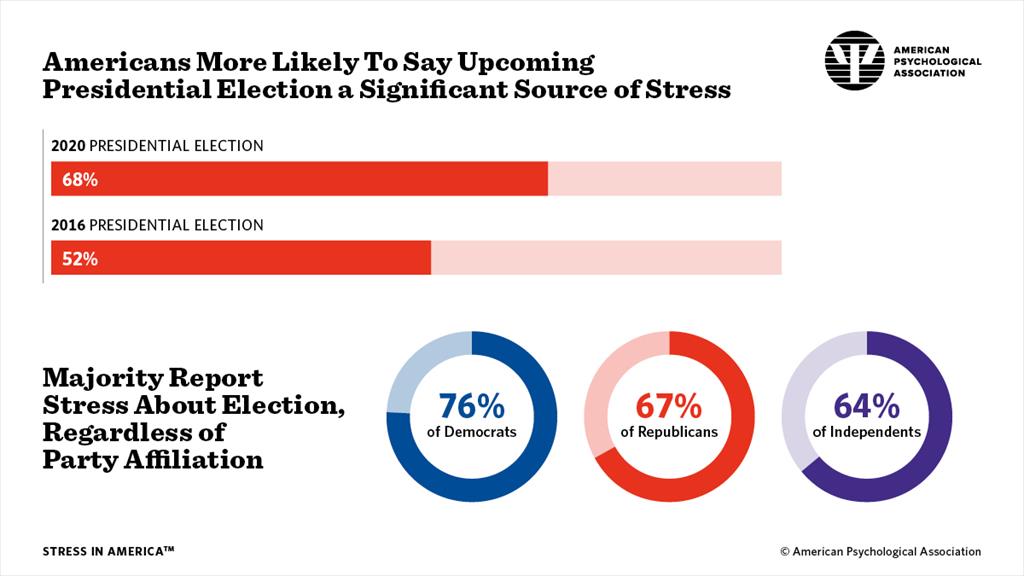
 Dr. Steven Stosny coined the term "election stress disorder” in 2016, with symptoms such as increased anxiety, insomnia, and difficulty concentrating. Dr. Stosny observed that "the pervasive negativity of political campaigns, amplified by the 24-hour news cycle and social media exposure," creates a significant level of stress, anxiety, or anger in many people. The American American Psychological Association (APA) Stress in America Survey found that more than two-thirds of U.S. adults (68%) say that the 2020 U.S. presidential election is a significant source of stress in their life. This is a substantial increase from the 2016 presidential election when 52% of US adults reported the same. “This has been a year unlike any other in living memory,” said Arthur C. Evans Jr., PhD, the APA's chief executive officer. “Not only are we in the midst of a global pandemic that has killed more than 200,000 Americans, but we are also facing increasing division and hostility in the presidential election. Add to that racial turmoil in our cities, the unsteady economy and climate change that has fueled widespread wildfires and other natural disasters. The result is an accumulation of stressors that are taking a physical and emotional toll on Americans.” The APA offers the following evidence-based advice to help people manage their stress related to the election:
This article by Scott Berinato of the HBR explores the different types of grief we are collectively experiencing in the face of this pandemic. There is a storm coming. There’s something bad out there. With a virus, this kind of grief is so confusing for people. Our primitive mind knows something bad is happening, but you can’t see it. This breaks our sense of safety. We feel the world has changed, and it has. We know this is temporary, but it doesn’t feel that way, and we realize things will be different. Just as going to the airport is forever different from how it was before 9/11, things will change and this is the point at which they changed. The loss of normalcy; the fear of economic toll; the loss of connection. This is hitting us and we’re grieving. Collectively. Finding ways to name what we are feeling, to speak it and ask for help, empowers us to experience and then move through the emotion. As the David Kessler states in the interview, “Emotion needs motion.” Kessler suggests grounding and mindfulness techniques to help calm overwhelming anxiety and re-center ourselves in the present and on the aspects of this situation which we can control.
|
About the AuthorClinical psychologist Dr. Kristy Novinski contributes insights, book and film reviews, discussions of pop culture, and exploration of news and research in the field of psychology. What I'm Reading
Categories
All
|
Las Colinas Psychological Services, PLLC |
© 2023 Las Colinas Psychological Services, PLLC. All rights reserved.
|







 RSS Feed
RSS Feed